It’s a relatively standard procedure
We’ll do all we can to save a healthy tooth, but extraction may be the best treatment option in some circumstances, such as:
- Fractured teeth.
- Severe gum disease.
- Trauma caused as the result of an accident.
- Complications when wisdom/third molars come in.
- Baby teeth that don’t fall out before adult teeth are cut.
- Extreme decay or infection that’s reached deep into a tooth.
- Crowding of your natural teeth, commonly followed by orthodontic treatment.
A filling, crown or root canal could be alternative treatment options, but where the damage is too severe to repair, your dentist might recommend an extraction.
How is a tooth extracted?
Your dentist will check through your medical history and, if required, take x-rays to reveal the length, shape and position of the tooth that needs to be extracted.
Using this information, they’ll be able to determine the best way to extract the tooth. In particularly complex cases, you may need to be referred to an oral surgeon, but most extractions can be completed routinely by your dentist.
There are two main types:
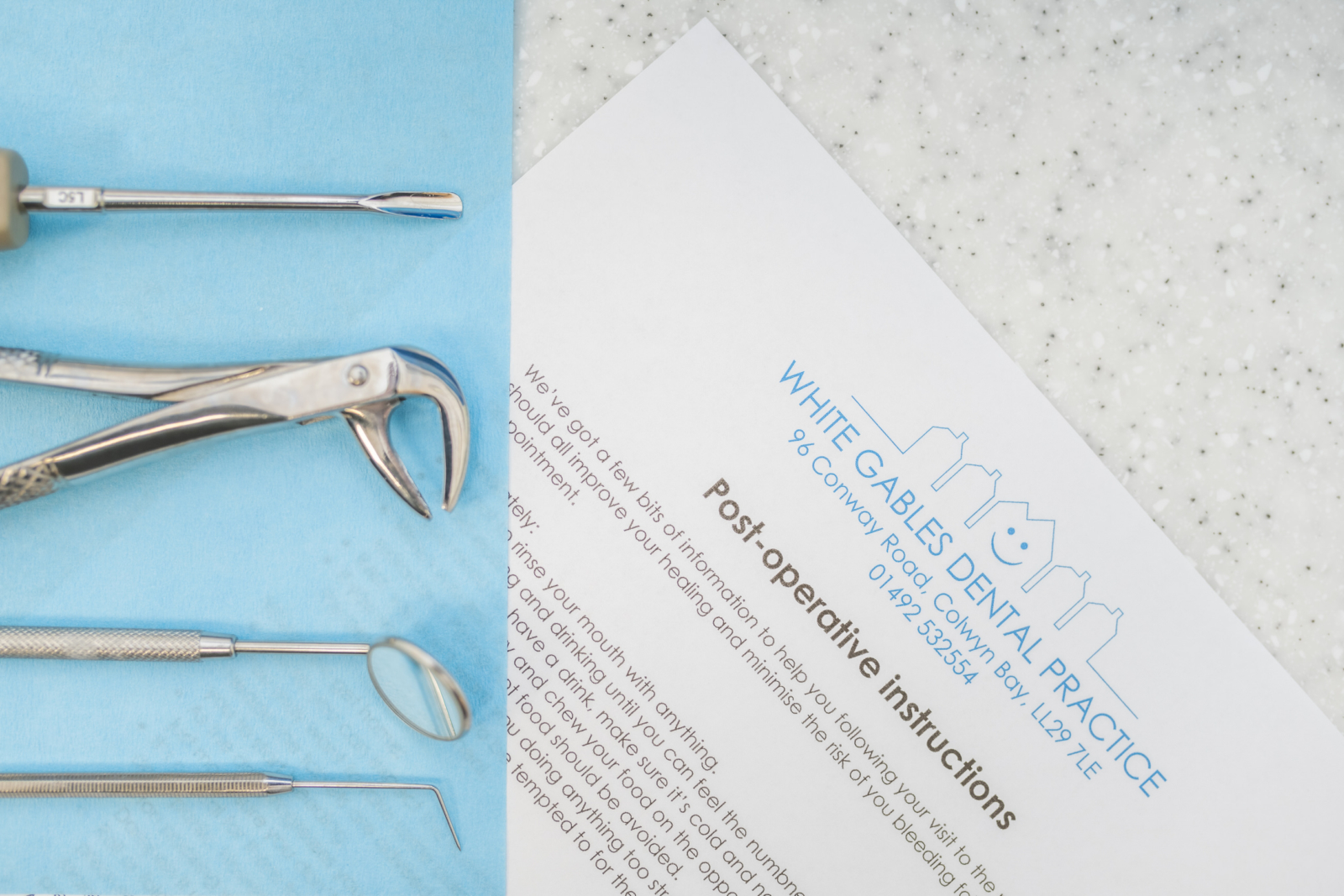
Simple extractions – a common procedure for a general dentist to complete, the area around the tooth will be numbed using local anaesthetic before the tooth is loosened using an elevator tool, and finally removed with dental forceps.
Surgical extractions – these may be completed by a general dentist or, in some circumstances, an oral surgeon. Removing a tooth that’s broken off close to the gumline, or hasn’t yet emerged, could involve making a small incision to the gum before the underlying tooth and roots can be extracted.
In either situation, anaesthetic will be used to make sure that you don’t experience any major discomfort during the extraction procedure. We tend to use local anaesthetic in our surgeries, but other dentist and surgeons may use intravenous drugs to sedate or fully anaesthetise a patient.
Once a tooth is removed, the socket may need to be thoroughly cleaned. In some situations, your dentist may place a dental bone graft, which helps to prevent any bone loss in your jaw. Stitches will be used where necessary, but often a simple piece of gauze and firm pressure is enough to stop any bleeding.
A blood clot will form in the socket, which is completely normal and should help the healing process.
Are there any risks?
There are potential risks with any surgical procedure, but a tooth extraction is quite a routine treatment for your dentist to complete. We will always go through pre-screening questions and give you relevant instructions before your treatment to help minimise any risk.
After a tooth has been extracted, you can expect light bleeding or swelling for up to 24 hours. Mild pain should be manageable with over-the-counter medication.
Longer term, the following could be complications:
- Post-surgical infection.
- Dry socket – where a blood clot fails to form in the socket.
- Nerve injuries.
- Tearing of the maxillary sinus.
- Slow healing.
In most cases, your mouth will recover within 48-72 hours, with your jaw slowly healing over a few weeks. That may mean you’ll need to wait a while before undertaking any further treatment in that area.
In cases where you’re suffering from infection, or pain from a broken tooth, a dental extraction can immediately ease your symptoms and remove harmful bacteria.
Aftercare tips you can follow
Your dentist will provide full instructions and answer any question you have, but here are some of the main things you’ll need to do post-extraction.
Apply firm pressure – you may be asked to bite down on a piece of dry sterile gauze for up to 30 minutes post extraction, just while a blood clot forms in the tooth socket.
Keep the area clean – this will help to prevent infection. For around 24 hours after your extraction avoid rising your mouth vigorously or cleaning the teeth next to the extraction site. It’s never advisable, but it could also affect your healing if you smoke during this period.
Take all medication as prescribed – this could include antibiotics to treat any lingering infection.
Avoid strenuous activity for at least 2 days – we don’t need much excuse to skip the gym, but having a tooth extracted is a legitimate reason.
Get a lift home – you could feel a little light-headed after having anaesthetic, so it’s a good idea for someone else to give you a lift home. If that’s not an option, you might like to take a bus, train, or taxi.
Choose softer foods – you might struggle with crunchy foods for a couple of days, so opt for soft things like pasta, rice, stew, yoghurt, or soups.
Avoid straws – sucking on a straw could cause blood clots to dislodge, potentially slowing down the heling process, or leading to a dry socket.
If you’ve got mild pain – you should be able to manage this at home using over-the-counter pain relief, such as paracetamol or ibuprofen.
If the pain or bleeding won’t stop – seek medical attention as soon as possible. You can contact us, but if you’re bleeding heavily you might need to go to A&E.
We’ll do all we can to make sure there aren’t any complications, but if you find you’re not healing, continue to have pain, or have any other dental issues, please get in touch with us. We’re here to help.
How much does a tooth extraction cost?
For a single tooth extraction, our costs are detailed below:
Private patients from: £125
With Denplan Essentials from: £112.50
With Denplan Care: covered
Filling the gap
Some people don’t mind having a gap, especially if it’s near the back of their mouth and doesn’t cause any issues with eating or speech.
However, your dentist will happily chat through your options if you’d like to explore filling the space left by your extracted tooth once everything has healed.
These could include a dental bridge, denture or implant.
Book for a more complete smile
Now you’ve had a chance to read about the treatments we can offer at White Gables Dental Practice, why not get in touch?